|
|||
The contribution of neuroimaging to the improvement of the quality of life of patients suffering from multiple sclerosis
VLAIKIDIS N.D.
A' Neurological Clinic of Aristotle University in Thessaloniki (Dir.: Prof. S. I. Baloyannis)
Summary From the Neuroimaging methods, the computerized axial tomography (CT) can reveal the existence of multiple sclerosis sometimes with pathognomic findings. The method of choice, however (especially during the first onsets), not only among the neuroimaging but also among all the other methods, is the magnetic resonance imaging (MRI). In its tomographic pictures of T2-Echo even the very small demyelinated foci are distinguished and they are enhanced with paramagnetic contrast medium, when they are active and a recent disturbance of blood-brain barrier exists.
This way, the MRI has the possibility of connecting the new symptoms with the new or enhanced foci and offers reliable data about the prognosis, determining in what areas the status is improved and where simultaneously worsened, while all the other biochemical or neurophysiological examinations interpret the algebraic sum of the continuous fight between improvement in some areas and simultaneous worsening in other regions of the nervous system, without disclosing where the improvement or the worsening takes place.
Neuroimaging helps MS-patients with the early diagnosis, the differential diagnosis from other illnesses with similar symptomatology, the prescription of the prognosis of illness, the documentation of the course of the illness, the answer to the dilemma if or when should a treatment be placed, the evaluation of effectiveness of applied medical treatment and the comprehensible information to the MS-patients, so that they will be able to cope with their illness and to help themselves better.
Key words: Multiple Sclerosis (MS), Quality of Life (QoL), Neuroimaging, MRI, CT.
Introduction
Multiple sclerosis (MS) is a chronic neurological disease that attacks young people, who have the most of their lives in front of them. Most cases are diagnosed between the ages of 20 and 40 and the induced disability aggravates the quality of life (QoL) of these patients for a long period of time1.
In the QoL-term there are many different meanings (depending on age, religion, nationality, mentality, education and other factors relating to the patients) included. Generally, in Greece, it is believed that QoL of the patients presents their ability to carry out their legal former actions and functions, which gave or enhanced the pleasure to live.
Neuroimaging helps MS-patients with the early diagnosis, the differential diagnosis from other illnesses with similar symptomatology, the prescription of the prognosis of the illness, the answer to the dilemma if or when should a treatment be applied, the documentation of the course of the illness, the evaluation of effectiveness of applied medical treatment and the comprehensible information of MS-patients, so that they will be able to cope with their illness and to help themselves better.
Material and method
Since the application of Magnetic Resonance Imaging (MRI) in Greece (1980), we have studied 355 patients suffering from MS. All these patients (except for the clinical, blood samples and neurophysiological examination) were also examined with Computer Tomography (CT) and MRI.
Many times even by the first event of the illness (paraplegia, hemiplegia, vertigo, walking instability, often double vision) serious disturbances in the functionality of the patient reducing the quality of their life can be caused.
The contribution of neuroimaging to the early diagnosis, to the differential diagnosis from other illnesses, that give similar clinical symptoms (e.g. syphilis, hysteria, AIDS, Lyme disease) is very important thanks to detailed depiction of the brain and spinal cord in vivo.
This information declares the correctness of the clinical diagnosis with objectivity and has the possibility of revealing subclinical improvements or deteriorations of the illness.
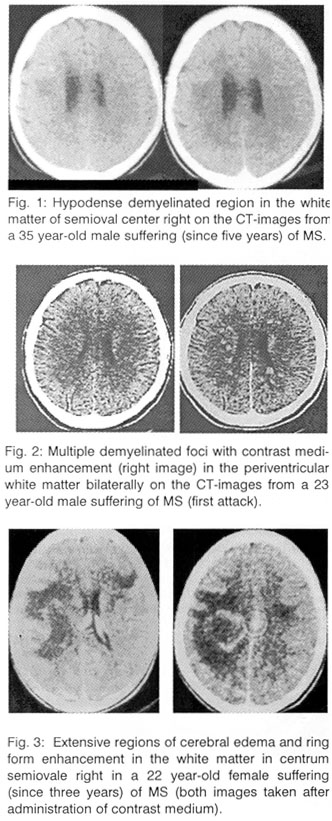
Among the Neuroimaging methods, the computerized axial tomography (CT) is able to reveal the existence of multiple sclerosis with pathognomic findings: in the chronic forms with relatively extensive hypodense periventricular regions without enhancement or space occupying action and at the onset or at the relapses of illness (Fig. 1), sometimes because of the disturbances of blood brain barrier, with small discrete hypodense periventricular foci, maybe with contrast medium enhancement (Fig. 2).
A repetition of CT two hours after intravenous injection of double dosage contrast medium (double-dose delayed CT scan) offers often many more diagnostic findings2,3.
Rarely - because of blood brain barrier breakdown - it is very likely that extensive regions of decreased density (with the same density of cerebral edema) and ring form enhancement are portrayed, like in a case of abscess, metastasis, glioma, parasitic illness and special inflammation of the brain (Fig. 3).
The method of choice, however, (especially during the first onsets), not only among the neuroimaging methods, but also among all other methods, is the magnetic resonance tomography (MRI, Fig. 4).
In the pictures of T2-Echo even the very small foci are distinguished as regions with signal of increased intensity in the white substance, particularly round the ventricular system of the brain, but also in the brain stem, in the spinal cord and in the optic nerve, which - when they are active and recent disturbance of blood-brain barrier exists - are enhanced with paramagnetic contrast medium (Fig. 5).
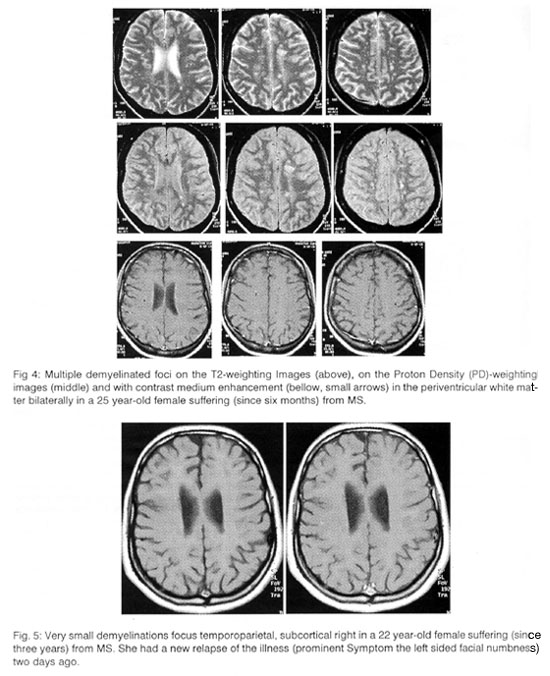
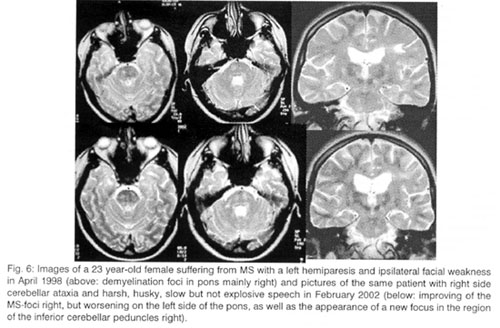
Therefore, the MRI has the possibility of clarifying the new symptoms, from which new foci are caused and offers reliable data about the prognosis, determining where the status is improved and where simultaneously worsened and if demyelinating foci exist in brainstem, while all other biochemical or neurophysiological examinations interpret the algebraic sum of the continuous fight of the improvement in some areas against the simultaneous worsening in other regions of the nervous system, without locating where the improvement or the worsening takes place (Fig. 6).
The offer of MRI to the differential diagnosis by the acute disseminated encephalomyelitis (ADEM), the Balo disease, the Lyme disease, the cerebral ischemia, the process of the cervical or the thoracic section of the spinal cord are usually, but not always, persuasive. In these cases, the contribution of the clinical information has the most important value to specify the correct diagnosis.
The offer of the positron emission tomography falls short regarding the offer of the magnetic tomography in the diagnosis of MS4; however, various optimizing methods of illustration, mainly in relation with MRI, have been devised and applied, such as the functional magnetic resonance imaging (fMRI), the magnetisation transfer imaging (ÌÔÉ) and mainly the magnetic resonance spectroscopy (MRS), which reveals the recent demyelinating activity with small reduction and the irreversible lesion with severe reduction of peak of N-aketylaspartate (NAA). At the same time, increase of inositol in the MRS reveals development of gliosis, while the increase of lipids and choline or choline to creatine ratio discloses significant demyelination5.
Discussion and conclusions
For the improvement of quality of life of patients with MS, the permanent unhindered collaboration of the patient, the doctor, the paramedical personnel (nurse, physiotherapist, psychologist, speech therapist) and the environment of the patient (familial, labour and social) is required. If this collaboration is not ideal, then the results of the confrontation of the illness will not be the best that could be possibly obtained.
The Neuroimaging and especially the MRI helps physicians notify patients about the diagnosis and prognosis of the illness, also in relation to Expanded Disability Status Scale [EDSS] score6. When patients are informed about the diagnosis of multiple sclerosis, they feel shocked and believe that they live in a nightmare that will finish soon. The pictures of MRI help to the objectification of this problem and the comprehension from the patients6,7. Most patients said that they were better off having received diagnostic information8.
Neuroimaging provides also reliable diagnostic clues to decide whether a therapy should be applied and, if yes, which therapy would be preferred.
If severe clinical kinetic deficits exist and the MRI reveals unfavourable prognostic signs (existence of demyelinating foci in the lower brain stem on in the spinal cord, which enhanced again, perifocal relapsing of cerebral edema at the same place by repeated exacerbations), then a therapy should be applied as soon as possible in order to avoid an axonal degeneration.
If, nevertheless, the MRI does not reveal demyelinating foci in the brain stem or in the spinal cord and the clinical picture is not characterized by heavy kinetic deficits (hemiplegia, paraplegia or tetraplegia) or is characterized by relatively heavy clinical deficits, which are being improved in some way, then it is believed, that the physician should follow the clinical course of the illness expecting a spontaneous remission and remyelination [without tiring (corporally and psychically) the patient with a maybe unnecessary therapy] and only intervene if it appears that there remains a significant degree of kinetic disability.
Anyway, because of the recently disclosed strong correlation between MRS-measures of axonal loss and disability in multiple sclerosis9-13, and the existing considerable consensus that axon damage occurs early in the course of multiple sclerosis14-19, it is believed, that the initiation of a immunomodulatory therapy in the early stage of the disease may be an important step to influence the natural unfavourable course of the disease.
In addition, after beginning with the therapeutic confrontation of the MS, the MRI also has the possibility of valuing the effectiveness of the therapy, revealing how much the number of the demyelination foci was decreased or not (always with very critical attention while keeping in mind that this reduction is maybe due to an automatic improvement of the illness).
If, however, the demyelination plaques are not decreased, despite the applying therapy, but remain or increase in number or in extent, then it is obvious that the treatment is not effective and that it should be modified.
Although the MRI is a more sensitive indicator than clinical assessment (active MRI-lesions are detected five to ten times more frequently than are the clinical exacerbations20), it is easier to quantify the MRI-changes than the clinical-changes and the MRI-assessments are more objective and reproducible than the clinical-assessments, the clinical Symptoms and course are the most important criteria for the management of the illness.
Still, more decisive is the contribution of MRI to the new proposed methods, such as the transplantation of cells of Schwann from peripheral nerves to the region of intracerebral MS-lesions (in Yale University, Connecticut, USA, with the hope that the cells of Schwann will survive and undertake the role oligodendrocytes in the function of remyelination, that has already been achieved on guinea-pigs21) or the transplantation of bone marrow cells in the human brain (hopping to generate new neurons and other types of brain cells22) locating the MS-lesions-targets for transplantation and checking the effectiveness of the methods with the disappearance or the reduction of the size of demyelination areas.
Also, the MRI is essential for the determination of the route and the destination of electrodes, for the realisation of new therapeutic techniques, as e.g. in the implantation of electrodes in the thalamus for the confrontation of the intense and, although treated with pharmacotherapy, not improved tremor that had been attempted in Vancouver23.
Last but not least, the MRI helps not only physicians notify patients about the diagnosis and prognosis of the illness (as it has already been reported), but also patients how they could help themselves better: With the precise knowledge of the localisation and the extent of the MS-lesions, there exists the possibility of convenient support of operations that are in danger.
Also, correct information helps patients place themselves positively to the illness, learning to live with MS. They must not feel ill or invalid, but permanently perform what the body can do, what the heart wishes and that the soul desires.
During the course of untreatable disease frequently the familiar environment gets tired, as time goes by, and apart from bodily, also psychical burden follows. Later, it is possible, that the same will happen with the patient's social environment, even with the paramedical and the medical personnel.
If this becomes perceptible from the patients, then they will be hurt immedicable and the deterioration of their situation will often be inevitable and irreversible.
These difficult hours we must remember, that a fellowman suffers, that we could be in their place and that we must feel the need to live and to follow the meaning of the phrase: Love Each Other!
REFERENCES
- Thompson, AJ: Clinical review of multiple sclerosis. Clin Immunother, 1996, 5 Suppl 1: p: 1-11.
- Weitze C, Hertel G, Brittner W: Multiple sclerosis: diagnostic value of computerized tomography with delayed scanning after a double-dose of contrast medium in comparison with other diagnostic tests. Neurosurg Rev 1988; 11(1):53-8.
- Poser CM, Kleefield J, O'Reilly GV, Jolesz F: Neuroimaging and the lesion of multiple sclerosis. AJNR Am J Neuroradiol. 1987 May-Jun; 8(3):549-52.
- Reiss J: New developments in neuroradiologic diagnosis. Indications for MRI and PET--advances in functional imaging. Fortschr Med 1998 Apr 20; 116(11):40-3.
- Paty DW and Moore W: Magnetic Resonance Imaging changes as living pathology in Multiple Sclerosis. In: Paty DW and Ebers GC: Multiple Sclerosis. F.A.Davis, Philadelphia, 1997; pp: 349-353.
- Bakshi R, Benedict RH, Bermel RA, Jacobs L: Regional brain atrophy is associated with physical disability in multiple sclerosis: semiquantitative magnetic resonance imaging and relationship to clinical findings. J Neuroimaging 2001 Apr; 11(2):129-36.
- Janardhan V, Bakshi R: Quality of life and its relationship to brain lesions and atrophy on magnetic resonance images in 60 patients with multiple sclerosis. Arch Neurol 2000 Oct; 57(10):1485-91.
- Mushlin AI, Mooney C, Grow V, Phelps CE: The value of diagnostic information to patients with suspected multiple sclerosis. Rochester-Toronto MRI Study Group. Arch Neurol 1994 Jan; 51(1):67-72.
- Matthews PM, De Stefano N, Narayanan S, Francis GS, Wolinsky JS, Antel JP, et al: Putting magnetic resonance spectroscopy studies in context: axonal damage and disability in multiple sclerosis. [Review]. Semin Neurol 1998; 18: 327-36.
- Grimaud J, Barker GJ, Wang L, Lai M, MacManus DG, Webb SL, et al: Correlation of magnetic resonance imaging parameters with clinical disability in multiple sclerosis: a preliminary study. J Neurol 1999; 246: 961-7.
- Paolillo A, Pozzilli C, Gasperini C, Giugni E, Mainero C, Giuliani S, et al: Brain atrophy in relapsing-remitting multiple sclerosis: relationship with 'black holes', disease duration and clinical disability. J Neurol Sci 2000; 174: 85-91.
- Fisher E, Rudick RA, Cutter G, Baier M, Miller D, Weinstock-Guttman B, et al: Relationship between brain atrophy and disability: an 8-year follow-up study of multiple sclerosis patients. Mult Scler 2000; 6: 373-7.
- Pelletier J, Suchet L, Witjas T, Habib M, Guttmann CR, Salamon G,et al: A longitudinal study of callosal atrophy and interhemispheric dysfunction in relapsing-remitting multiple sclerosis. Arch Neurol 2001; 58: 105-11.
- Medana IM, Esiri MM: Axonal damage: a key predictor of outcome in human CNS diseases. Brain 2003, 126, 515-530.
- Ferguson B, Matyszak MK, Esiri MM, Perry VH: Axonal damage in acute multiple sclerosis lesions. Brain 1997; 120:393-9.
- Trapp BD, Peterson J, Ransohoff RM, Rudick R, Mork S, Bo L: Axonal transection in the lesions of multiple sclerosis. New Engl J Med 1998; 338: 278-85.
- Bitsch A, Schuchardt J, Bunkowski S, Kuhlmann T, Bruck W: Acute axonal injury in multiple sclerosis. Correlation with demyelination and inflammation. Brain 2000; 123: 1174-83.
- Kornek B, Storch MK, Weissert R, Wallstroem E, Stefferl A, Olsson T, et al: Multiple sclerosis and chronic autoimmune encephalomyelitis: a comparative quantitative study of axonal injury in active, inactive, and remyelinated lesions. Am J Pathol 2000; 157: 267-76.
- Kuhlmann T, Lingfeld G, Bitsch A, Schuchardt J, Bruck W: Acute axonal damage in multiple sclerosis is most extensive in early disease stages and decreases over time. Brain 2002; 125: 2202-12.
- Goodkin DE, Rudick RA, Ross JS. The use of brain magnetic resonance imaging in multiple sclerosis. Arch Neurol 1994;51(5):505-516.
- Stangel M: Transplantation of myelinating cells as regenerative therapy for multiple sclerosis - experimental basis and present state of clinical studies. Nervenarzt 2002 Oct; 73(10):937-45.
- Mezey E, Key S, Vogelsang G, Szalayova I, Lange GD, Crain B: Transplanted bone marrow generates new neurons in human brains. Proc Natl Acad Sci U S A 2003 Feb 4; 100(3):1364-9.
- Berk C, Carr I, Sinden M , Martzke I, Honey CR: Thalamic deep brain stimulation for the treatment of tremor due to multiple sclerosis: a prospective study of tremor and quality of life. I Neurosurg 2002 Oct;97(4):815-20.
